Cataract surgery complications and side effects
Cataract surgery complications are few, and cataract surgery is among the most common and most successful surgical procedures performed today.
In the United States, about 4 million cataract surgery procedures are performed every year.
Cataract surgery is very safe. One study of more than 221,000 cataract surgery patients showed that 99.5% of the patients had no serious complications following their procedure.
Research also showed that the risk of severe complications decreased significantly with advances in surgical tools and techniques over the 12-year period during which the surgeries were performed.
When cataract surgery complications do occur, they can include:
Posterior capsule opacification (PCO)
Intraocular lens dislocation
Eye inflammation
Photopsia (perceived flashes of light)
Macular edema (swelling of the central retina)
Ptosis (droopy eyelid)
Ocular hypertension (elevated eye pressure)
When cataract surgery complications occur, most are minor and can be successfully treated medically or with additional procedures.
Posterior capsule opacification (PCO)
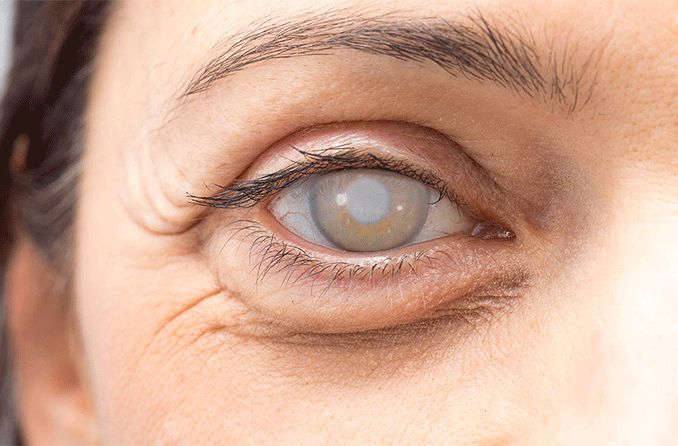
One of the most common cataract surgery complications is a posterior capsule opacification. This can also be called posterior capsule opacity, or PCO for short.
Although some people call posterior capsule opacification a "secondary cataract," it isn't really a cataract. Once a cataract is removed, it doesn't come back.
During cataract surgery, your surgeon will remove the cloudy natural lens of your eye (the cataract) and replace it with a clear intraocular lens (IOL) implant. Much of the thin clear membrane that surrounds the natural lens (called the lens capsule) is left intact during surgery, and the IOL is usually implanted within it.
When the cataract is removed, your surgeon makes every attempt to maintain the integrity of the lens capsule, and normally your vision after cataract surgery should be very clear.
However, in some cases, the posterior (back) portion of the lens capsule becomes hazy over time, causing blurry vision. This process can occur within months or years after cataract surgery.
An analysis of several studies found that posterior capsule opacification occurred in 11.8% of patients at one year after cataract surgery, in 20.7% at 3 years, and in 28.4% at 5 years.
In some cases, the condition can progress significantly and treatment is required to restore clear vision.
Treating posterior capsule opacity
Fortunately, a YAG laser can treat posterior capsule opacity safely, effectively and painlessly. This procedure, known as YAG laser capsulotomy, can often be performed in your cataract surgeon's office.
YAG laser capsulotomy involves just a few simple steps:
The eye is usually dilated with dilating eye drops before the procedure.
A laser removes the hazy posterior capsule from your line of sight without making an incision or "touching" the eye.
Many ophthalmologists will recommend anti-inflammatory eye drops following the procedure.

A procedure called a YAG laser capsulotomy can quickly restore vision following posterior capsular opacification.
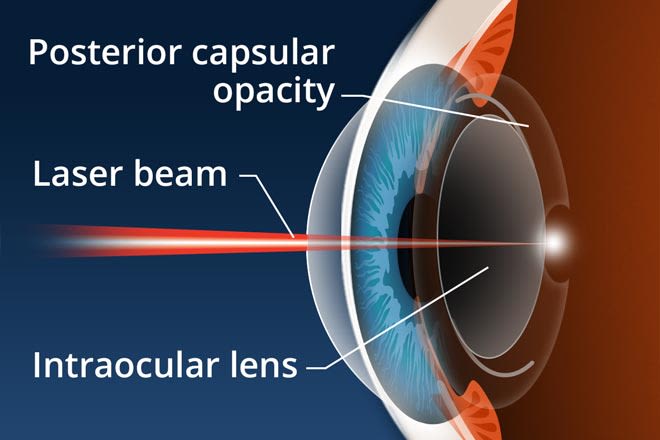
A laser capsulotomy is a relatively simple, in-office procedure that takes only a few minutes. A laser beam is directed at the cloudy capsule behind the intraocular lens (IOL) and the energy from the laser vaporizes the tissue, restoring clear vision.
This process takes only a few minutes and is entirely painless, both during and after the procedure.
You will need to remain still during the procedure. Some patients, such as children or those with mental disabilities, may need to be sedated.
Following a YAG laser capsulotomy, you may resume normal activities immediately. You may experience some floaters afterward, but these should resolve within a few weeks.
Most people can expect their vision to improve within a day. As with any eye procedure, however, call your eye doctor immediately if vision worsens or fails to improve.
Because the YAG laser removes the central zone of the cloudy posterior capsule behind the intraocular lens, the condition cannot return. Only one laser treatment is required to permanently eliminate vision loss caused by posterior capsule opacification after cataract surgery.
YAG laser capsulotomy risks
Although a YAG laser capsulotomy poses slight additional risk, the procedure is extremely safe overall.
The most notable risk is a small chance that the retina separates from the inner back of the eye. This is called retinal detachment.
Statistics suggest that the lifetime risk of a detached retina as a cataract surgery complication in the United States is about 1%. That number rises to about 2% after YAG laser capsulotomy. It is important to be aware of this cataract surgery risk.
Dislocated intraocular lenses
Another example of a cataract surgery complication is a malpositioned or dislocated intraocular lens. You may see the edge of the lens implant, or you may even develop double vision. If the intraocular lens becomes too badly dislocated, your visual acuity could decrease substantially.
How can the lens become malpositioned or dislocated?
In most cataract surgeries, the intraocular lens is placed inside the "capsular bag," which contains the cloudy natural lens or cataract of the eye.
Ophthalmologists make every attempt to maintain the integrity of the capsular bag so that the intraocular lens can be positioned correctly within it. But the capsular bag is extremely thin — approximately the thickness of a single red blood cell — and can sometimes rupture or break.
The capsular bag itself may also dislocate due to weakness or breakage of the fibers that hold it in place. This condition places you at risk of malpositioning or dislocation of the lens implant.
Even without underlying complications, intraocular lenses can still dislocate — especially if one of the springy "arms" holding the lens in place is positioned improperly inside the capsular bag or becomes malpositioned later on.
When an intraocular lens implant is malpositioned or dislocated, your cataract surgeon can probably reposition it in a second procedure. In some cases, the lens implant must be sewn in place, or another type of lens must be implanted.
If IOL dislocation occurs following a recent cataract surgery, repositioning the lens should be done soon. This is because lens implants begin to "scar" into place approximately three months after original implantation and can become much more difficult to remove.
The risk of IOL dislocation after cataract surgery is very low. One study found that it occurred in only 0.1% of patients in the 10 years following surgery and in 0.7% within 20 years.
If you do experience a malpositioned or dislocated intraocular implant, your chances of a good outcome following a second procedure are very good if you and your surgeon take action promptly.
Cataract surgery side effects
Other potential cataract surgery side effects range from minor eye inflammation to serious vision loss.
Minor side effects can include:
Swelling of the cornea or retina
Increased pressure in the eye (ocular hypertension)
Droopy eyelid (ptosis)
These minor complications usually clear up with medications and more healing time.
The risk of severe vision loss is very low. When this occurs, it's often as a result of bleeding or an infection inside the eye.
Some cataract surgery complications occur quite a while after surgery. For example, a detached retina can occur months or years after a perfectly successful cataract procedure.
Most patients with retinal detachment have a good outcome if they see their ophthalmologist when symptoms first begin and treatment is done immediately. However, a small percentage will have substantially and permanently reduced vision.
Be sure to report floaters, flashes of light and any curtain-like vision loss to your ophthalmologist immediately. These can be symptoms of a retinal detachment.
Vision after cataract surgery
If you have any problem with sensitivity to sunlight after cataract surgery, eyeglasses with photochromic lenses, which darken automatically to UV rays, can often provide relief.
Also, for residual refractive error and presbyopia after surgery, progressive lenses with anti-reflective coating may be able to sharpen your vision for activities like night driving and reading.
People whose vision fails to improve after cataract surgery often have underlying eye disorders, such as age-related macular degeneration, diabetic retinopathy and other eye conditions.
Some of these individuals may benefit from other procedures or from low vision aids.
READ NEXT: Refractive cataract surgery
Future of cataract surgery seems promising. Ocular Surgery News. February 2021.
Severe adverse events after cataract surgery among Medicare beneficiaries. Ophthalmology. June 2011.
A systematic overview of the incidence of posterior capsule opacification. Ophthalmology. July 1998.
Risk of late intraocular lens dislocation after cataract surgery, 1980–2009: A population-based study. American Journal of Ophthalmology. October 2011.
Page published on Wednesday, February 27, 2019